PREVNAR 7#
PREVNAR 7 (PCV7) was the first pneumococcal conjugate vaccine licensed in the United States in February 2000. It contained purified capsular polysaccharides from seven serotypes of Streptococcus pneumoniae (4, 6B, 9V, 14, 18C, 19F, and 23F) individually conjugated to CRM₁₉₇ carrier protein. These seven serotypes accounted for approximately 80% of invasive pneumococcal disease in children under 6 years of age in the U.S. prior to vaccine introduction. The vaccine was designed to elicit T-cell dependent immune responses in infants and young children, unlike the 23-valent polysaccharide vaccine which is ineffective in this age group. PCV7 was replaced by Prevnar 13 in 2010 and is no longer produced.
Mechanism of Action#
What the Mechanism Affects#
Prescribed For#
- Invasive Pneumococcal Disease: Active immunization against invasive disease (bacteremia, meningitis) caused by S. pneumoniae serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F in infants and toddlers. Routine schedule: 2, 4, 6, and 12-15 months of age.
- Acute Otitis Media: Active immunization against otitis media caused by vaccine serotypes, though efficacy was only 6-7% against all causes of otitis media and 57% against vaccine-serotype otitis media.
Contraindications & Warnings#
Absolute Contraindications & Major Precautions
Adverse Effects Profile#
Common Side Effects (Clinical Trials)#
- Injection Site Reactions: Erythema/redness (10-14%), induration (10-12%), tenderness (17.9-23.3%), interfered with limb movement (3.1-9.2%)
- Fever: ≥38.0°C (15.1-33.6%), >39.0°C (0.9-3.8%). Greater with concurrent DTaP administration. Most common after dose 2.
- Systemic Events – Infants: Irritability (48-65.3%), drowsiness (25.6-50.8%), restless sleep (15.3-25.2%), decreased appetite (17-20.7%)
- Gastrointestinal: Vomiting (10.4-16.8%), diarrhea (8.3-11.9%)
- Urticaria-like Rash: 0.4-1.4% within 48 hours; 1.3-6% from 3-14 days post-vaccination, most often after 4th dose when given with MMR
Serious Adverse Effects#
- Deaths & SIDS: 12 deaths occurred among Prevnar recipients in clinical trials (5 SIDS, 7 with alternative causes) through April 1999. Control group had 21 deaths (8 SIDS, 12 alternative causes, 1 SIDS-like death). SIDS rates were similar to or lower than California state data, but temporal associations raise concerns.
- Seizures: 8 Prevnar recipients vs 4 control recipients had seizures within 3 days of immunization (October 1995-April 1998). 7 of 8 Prevnar cases received concurrent DTP vaccines. One additional seizure reported in ancillary studies.
- Hypotonic-Hyporesponsive Episode (HHE): 1 case in efficacy study, 2 additional cases in other studies—all occurred with concurrent DTP vaccines. Serious neurological reaction.
- Anaphylaxis/Hypersensitivity: Anaphylactic/anaphylactoid reactions including shock, face edema, dyspnea, bronchospasm reported post-marketing. Life-threatening.
- Hospitalizations Within 3 Days: 24 hospitalizations (29 diagnoses) among 17,066 subjects. Diagnoses included bronchiolitis (5), congenital anomaly (4), pneumonia (2), febrile seizure (1), and others.
- Emergency Room Visits: 162 visits (182 diagnoses) within 3 days including febrile illness (20), gastroenteritis (19), otitis media (15), viral syndrome (10), febrile seizure (3).
- Post-Marketing: Injection site dermatitis/urticaria/pruritus, lymphadenopathy, angioneurotic edema, erythema multiforme, crying, apnea (especially in premature infants).
Drug Interactions#
IMPORTANT DISCLAIMER: These drug interactions are based on the vaccine insert referenced clinical trials and may not include data outside of that window. Therefore, lack of safety studies should not be considered evidence for safety and you are encouraged to research for yourself.
Active & Inactive Ingredients#
Each 0.5 mL dose of PREVNAR 7 contained the following components:
Active Substances (Per 0.5 mL Dose)#
- Polysaccharide Serotypes 4, 9V, 14, 18C, 19F, 23F: 2 µg each (conjugated to CRM₁₉₇)
- Polysaccharide Serotype 6B: 4 µg (conjugated to CRM₁₉₇)
- Total Saccharide Content: 16 µg per dose
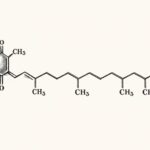
- CRM₁₉₇ Carrier Protein: Approximately 20 µg per dose (diphtheria toxin variant isolated from Corynebacterium diphtheriae strain C7 (β197), grown in casamino acids and yeast extract-based medium, purified through ultrafiltration, ammonium sulfate precipitation, and ion-exchange chromatography)
Manufacturing Process#
- Each serotype grown in soy peptone broth
- Polysaccharides purified through centrifugation, precipitation, ultrafiltration, and column chromatography
- Chemically activated to create saccharides
- Directly conjugated to CRM₁₉₇ protein carrier through reductive amination
- Individual glycoconjugates purified and analyzed for saccharide:protein ratios, molecular size, free saccharide, and free protein
Adjuvant#
- Aluminum Phosphate: 0.125 mg aluminum per 0.5 mL dose (neurotoxic heavy metal, accumulates in brain tissue, linked to developmental delays, autoimmune conditions, and neurological damage)
Physical Characteristics#
- Manufactured as liquid preparation
- After shaking: homogeneous white suspension
- MUST SHAKE VIGOROUSLY immediately prior to use to obtain uniform suspension
- No preservatives listed in original formulation
Important Note: The package insert states potency is determined by quantification of each saccharide antigen and saccharide-to-protein ratios. All polysaccharides were chemically activated and covalently bound to CRM₁₉₇ through reductive amination, creating glycoconjugates designed to trigger T-cell dependent immune responses.
Clinical Trials & Efficacy#
Primary Efficacy Study (Northern California Kaiser Permanente)#
Design: Randomized, double-blind trial (October 1995-August 1998). 37,816 infants randomized: 18,906 received Prevnar, 18,910 received control (investigational meningococcal C conjugate vaccine). Doses at 2, 4, 6, and 12-15 months.
Because there was no placebo group and the control group received another vaccine that itself had never been tested against a placebo, the results of these studies cannot demonstrate safety or efficacy. To prove efficacy and safety you need trials that have placebos which can compare mortality and severity not simply cases.
- Invasive Disease Due to Vaccine Serotypes:
- Per protocol (≥14 days after dose 3): 0 Prevnar cases vs 17 control cases = 100% efficacy (95% CI: 75.4-100%)
- Intent-to-treat: 0 Prevnar cases vs 22 control cases = 100% efficacy (95% CI: 81.7-100%)
- All 22 control cases were bacteremic; additional diagnoses: meningitis (2), pneumonia (2), cellulitis (1)
- All Invasive Pneumococcal Disease (any serotype):
- Per protocol: 2 Prevnar cases vs 20 control cases = 90% efficacy (95% CI: 58.3-98.9%)
- Intent-to-treat: 3 Prevnar cases vs 27 control cases = 88.9% efficacy (95% CI: 63.8-97.9%)
- Extended Follow-up (to April 20, 1999):
- Per protocol: 1 Prevnar case vs 39 control cases
- Intent-to-treat: 3 Prevnar cases vs 49 control cases
- Similar efficacy estimates maintained
Otitis Media Efficacy#
Finnish Trial: 1,662 infants randomized to Prevnar or Hepatitis B vaccine (control) at 2, 4, 6, 12-15 months. Parents brought children for respiratory infections or AOM symptoms. Tympanocentesis performed if AOM diagnosed; middle ear fluid cultured.
- AOM Due to Vaccine Serotypes: 57% efficacy per protocol (95% CI: 44-67%), 54% ITT (95% CI: 41-64%)
- All Culture-Confirmed Pneumococcal AOM: 34% efficacy per protocol (95% CI: 21-45%), 32% ITT (95% CI: 19-42%)
- Vaccine-Related Serotypes (6A, 9N, 18B, 19A, 23A): 51% efficacy per protocol (95% CI: 27-67%), 44% ITT (95% CI: 20-62%)
- CRITICAL FINDING – Serotype Replacement: Vaccine efficacy against non-vaccine serotype AOM was -33% per protocol (95% CI: -80 to 1) and -39% ITT (95% CI: -86 to -3), indicating vaccinated children had INCREASED risk of otitis media from non-vaccine serotypes
- All AOM Episodes (any cause): Only 6% reduction per protocol (95% CI: -4 to 16, not statistically significant), 4% ITT (95% CI: -7 to 14, not significant)
NCKP Trial Otitis Media Assessment: 34,146 infants (October 1995-April 1998). Physician visits for otitis media identified by coding. No tympanocentesis, no standard definition.
- All Otitis Media Episodes: Only 7% reduction per protocol (95% CI: 4-10%), 6% ITT (95% CI: 4-9%)
- Recurrent AOM (3 episodes in 6 months or 4 in 12 months): 9% reduction in both per protocol and ITT (95% CI: 3-15 and 4-14)
- Tympanostomy Tube Placement: 20% reduction per protocol (95% CI: 2-35%), 21% ITT (95% CI: 4-34%)
Immunogenicity Data#
- Significant antibody response to all 7 vaccine serotypes following 3 or 4 doses
- Geometric mean concentrations varied among serotypes
- 91.4-100% achieved functional antibody (OPA titer ≥1:8) after primary series
- Minimum protective antibody level NOT established for any serotype against invasive disease or otitis media
- Induces functional opsonophagocytic antibodies after 3 doses
Critical Analysis: While PREVNAR 7 appeared to demonstrate excellent efficacy (97-100%) against invasive disease caused by vaccine serotypes, the real-world impact was limited. The vaccine covered only 7 of ~90 pneumococcal serotypes. Otitis media efficacy was marginal at best—only 6-7% reduction in total AOM episodes despite being a stated indication. The Finnish trial documented concerning serotype replacement with increased non-vaccine serotype infections. Post-marketing surveillance confirmed this phenomenon, with serotype 19A (not in PCV7) becoming dominant and more antibiotic-resistant. The vaccine prevented approximately 80% of invasive disease in the pre-vaccine era, but serotype replacement reduced this benefit over time, leading to replacement with Prevnar 13 in 2010. No placebo-controlled safety studies were conducted—control was another investigational vaccine (meningococcal C conjugate), making it impossible to assess true vaccine safety profile.
Critically, while these vaccines tend to show high “efficacy” against their targeted serotypes in clinical trials, this effect diminishes over time not only because of serotype replacement—where non-vaccine serotypes become dominant in vaccinated populations—but also because vaccine-induced immunity itself wanes. In contrast, natural infection covers all serotypes and provides more robust immunity over time.
Sources: Prevnar Package Insert (Wyeth Pharmaceuticals); Black S, et al. Pediatr Infect Dis J. 2000;19:187-195; Eskola J, et al. N Engl J Med. 2001;344:403-409; CDC MMWR 2000.
Vitamins & Minerals Affected#
PREVNAR 7, containing aluminum adjuvant and multiple bacterial antigens, affects nutrient status and metabolic processes through immune activation and oxidative stress:
Impact: Vitamin C rapidly depleted during immune challenges. Infants have limited reserves. Depletion impairs immune function, collagen synthesis, wound healing, and antioxidant defense. Critical during 2-6 month vaccination period when reserves are lowest.
Impact: Depletes glutathione, cysteine, methionine. Impairs detoxification pathways. Children with MTHFR variants, GST deletions, or compromised glutathione synthesis at substantially higher risk of adverse effects and aluminum accumulation.
Impact: Magnesium essential for 300+ enzymatic reactions, neurotransmitter synthesis, nerve conduction, muscle function. Depletion causes irritability, sleep disturbances, muscle tension, neurological symptoms—commonly reported post-vaccination effects.
Impact: Essential for immune function, thymic development, T-cell maturation, DNA synthesis, growth. Transient but significant depletion during critical developmental period (2-6 months). Can impair subsequent immune responses.
Impact: Critical for neurotransmitter synthesis (serotonin, dopamine, GABA), DNA methylation, homocysteine metabolism, myelin formation. Depletion during rapid brain development (first year of life) can affect neurological outcomes. MTHFR variants increase vulnerability.
Impact: Critical for protecting against oxidative damage, thyroid hormone metabolism, immune function. Deficiency increases susceptibility to vaccine-induced oxidative stress. Geographic variations in soil selenium affect baseline status.
Impact: Depletion increases membrane permeability, potentially affecting blood-brain barrier integrity. Works synergistically with vitamin C and selenium—depletion of one affects others.
Impact: Essential for bone development, muscle contraction, nerve transmission, cellular signaling. Disruption during infancy can affect skeletal development and neurological function.
Recommendations for Parents
- Pre-Vaccination Optimization: Ensure optimal nutritional status before vaccination, particularly vitamin C, magnesium, zinc, and B-vitamins.
- Post-Vaccination Support: Consider antioxidant and mineral supplementation for 7-14 days post-vaccination, especially for multiple simultaneous vaccines.
- Breastfeeding: Exclusive breastfeeding provides protective antibodies and nutrients. Mothers should optimize their own nutrient intake.
- Genetic Testing: Children with MTHFR variants, glutathione synthesis defects, or family history of vaccine reactions may benefit from enhanced nutritional support.
- Monitor Symptoms: Unusual irritability, sleep disturbances, developmental regression, or prolonged fever may indicate nutrient depletion or adverse reaction.
- Spacing: Avoid simultaneous administration of multiple vaccines to reduce cumulative aluminum burden and nutrient demands. Consider avoiding.
Note: These effects are based on established immunological, toxicological, and biochemical principles. Individual responses vary significantly based on baseline nutritional status, genetic polymorphisms (especially MTHFR, GST, metallothionein genes), gut health, concurrent illnesses, and number of simultaneously administered vaccines. The standard ACIP schedule recommends Prevnar 7 be given with DTaP, Hib, Hepatitis B, and IPV—potentially 5-6 antigens plus multiple aluminum doses in one visit. This dramatically increases nutrient demands and oxidative stress. Consultation with a knowledgeable healthcare provider or integrative pediatrician is strongly recommended, particularly for high-risk children.
IMPORTANT DISCLAIMER: This information is for educational purposes. Prevnar 7 is no longer manufactured (discontinued 2010, replaced by Prevnar 13). This analysis is based on the original formulation’s documented ingredients and known biochemical interactions. Parents considering current pneumococcal vaccines should request ingredient lists and research current formulations.