Tylenol is an Acetaminophen, whereas Aspirin is an NSAID (nonsteroidal anti-inflammatory drug). We have already discussed the dangers of aspirin, including its association with brain hemorrhaging and increased mortality when taken regularly. However, Tylenol takes this a step further as the more deadly agent and is far more dangerous, as will be demonstrated.
In 1955, McNeil Laboratories—purchased four years later by Johnson & Johnson—created the Tylenol brand. The following year, Tylenol became available over the counter and has since grown into the most prescribed pain medication.
Johnson & Johnson portrays itself as a “family company,” but this image is entirely false. Over the past forty years, the company has repeatedly been cited for health and safety violations as well as workplace violations, including incidents involving contaminated Tylenol containing Burkholderia cepacia, a bacterium resistant to antibiotics. It was later claimed that the contamination was not found in the capsules themselves but only in the storage drums, followed by a report issued by the corrupt CDC stating that “Burkholderia cepacia is not likely to cause health problems for those with healthy immune systems.” Had this contamination been found in an herbal supplement, the response would have been drastically different.
What is Tylenol prescribed for?#
Fever –Tylenol was originally marketed as an antipyretic to reduce fever in both children and adults, despite the fact that neither its long-term safety nor its true efficacy has ever been conclusively proven. Fever is not a disease; it is a protective, immune-driven response designed to inhibit pathogens and accelerate healing. Suppressing this process does not resolve the underlying cause and will prolong illness while placing unnecessary stress on the liver. (See the Side Effects section for a deeper explanation of this danger.)
Pain – Extra Strength Tylenol is routinely prescribed for pain relief and is even administered intravenously in certain emergency departments. This practice persists despite limited to no high-quality evidence demonstrating meaningful analgesic benefit. Tylenol does not address the source of pain, inflammation, or tissue damage; it merely dulls perception while allowing the underlying pathology to progress unchecked.
Osteoarthritis – The American College of Rheumatology has recommended Tylenol as a treatment option for osteoarthritis of the hip, hand, and knee. However, later and more rigorous studies demonstrated that Tylenol provides only a minimal benefit—so small that it is not logically defensible when weighed against its well-documented risks and side effects.[1]Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomized placebo-controlled trials
Back Pain –The same meta-analysis concluded unequivocally that Tylenol is “ineffective in the treatment of low back pain.” Despite this finding, it continues to be prescribed as a first-line intervention, offering false reassurance while doing nothing to resolve muscular imbalance, inflammation, nerve irritation, or structural dysfunction.
Headaches – Tylenol is commonly recommended for tension headaches and migraines, even though headaches are often driven by the inflammatory process in response to a problem, dehydration, mineral deficiencies, hormonal imbalance, or vascular dysfunction. Tylenol addresses none of these causes. Repeated use for headaches increases the risk of rebound headaches and cumulative liver toxicity, creating a cycle of dependency with no resolution.
Dental Procedures – Dentists frequently recommend Tylenol following extractions, root canals, and other procedures under the assumption that it is “gentler” than alternatives. Tylenol does not meaningfully reduce inflammation, swelling, or tissue trauma and instead exposes patients to hepatotoxic risk during a period when the body is actively attempting to heal.
Across all of these indications, Tylenol is prescribed not because it is effective, but because it is familiar, normalized, and aggressively marketed. It suppresses symptoms without addressing the cause, interferes with natural healing mechanisms, and exacts its cost silently through liver and other organ damage that is often dismissed—until it is irreversible.
How does Tylenol work on the body?#
According to the American Chemical Society “researchers don’t know how the popular painkilling medicine in Tylenol works”[2]How Does Acetaminophen Work? Researchers Still Aren’t Sure – The article goes on to explain that what we do know is that it is very toxic to the liver, but we are not sure the process by which it works or completely how it works on the body. This is a SERIOUS issue. One of the issues brought up in this article is that the difference between a “safe dose” and “toxic dose” is a very fine line which could easily lead to permanent liver damage or even death.
What we do know!
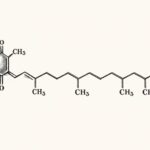
Researchers believe that acetaminophen (Tylenol) blocks cyclooxygenase (COX) enzymes which play a role in forming prostaglandins, which are pain and inflammation-mediating signaling molecules. If this is true (we do not know) then it acts in a similar fashion to Aspirin. But we know that even if this is true that it has other processes on the body which Aspirin does not.
Medicinenet states that while the exact mechanism of Tylenol is unknown it elevates the pain threshold so that you for instance what used to be a level 10 pain now feels like a level 7 perhaps. This is dangerous because it DOES NOT PROVIDE ANY HEALING so you aren’t fixing the problem but simply masking it while damaging your liver. On top of this Tylenol manipulates the bodys wonderful temperature regulating system called the Hypothalamus. The Hypothalamus triggers a fever to protect and heal the body, it is a NECESSARY process that Tylenol manipulates and negatively effects. We do not know if Tylenol may permanently damage the Hypothalamus which could lead to serious health concerns currently not tagged to Tylenol.
Tylenol – the drug of lies!#
Tylenol/Antipyretics Suppress Antibody Response to Virus
In a human study of volunteers infected with rhinovirus, the use of antipyretics like Tylenol was associated with suppression of serum antibody response, increased symptoms and ZERO decrease in shedding. The study concluded that while there was no significant difference the Tylenol treated group had a “trend toward longer duration of virus shedding”[3]Adverse effects of aspirin, acetaminophen, and ibuprofen on immune function, viral shedding, and clinical status in rhinovirus-infected volunteers.
Yup, you read that right! Taking Tylenol INCREASES your duration of virus. But wait… this is not an isolated case. This drug is prescribed for THOUSANDS of symptoms it does NOTHING POSITIVE for.
Tylenol: more harm than good for chickenpox?
In a study of 72 children between the ages of 1-12 years of age 31 received placebo and 37 received Tylenol in treatment of chickenpox. Wait for it… the placebo group excelled over the Tylenol group to scabbing by almost a whole day. The researchers conclude “These results provide evidence that acetaminophen does not alleviate symptoms in children with varicella[Chickenpox] and may prolong illness.”[4]Acetaminophen: more harm than good for chickenpox
Preventing Febrile Convulsions/Seizures in Children
It is a huge myth that Tylenol is beneficial for children prone to febrile convulsions during fever, in fact there is great evidence to suggest that administration of Tylenol INCREASES the chances of recurrence while providing no benefit. Several studies indicate that allowing the fever to reach 40 degrees Celsius decreases the chances of Febrile Convulsion recurrence so consequently hindering that fever would inevitably increase the risk of recurrence. Also it has been found that certain risk factors are present in whether a child will have FS and Tylenol does NOT improve or benefit these at all. Many studies find no benefit to Tylenol over placebo in treatment of FS.[5]Randomized, controlled trial of ibuprofen syrup administered during febrile illnesses to prevent febrile seizure recurrences. Pediatrics. 1998;102:E51. [6]A study of the efficacy of antipyretic drugs in the prevention of febrile seizure recurrence. [7]Lower degree of fever at the initial febrile convulsion is associated with increased risk of subsequent convulsions. [8]Paracetamol for treating fever in children.
Side Effects & Statistics#
Acetaminophen toxicity is repeatedly identified as the most common cause of acute liver failure in the United States. It is associated with roughly 56,000 emergency department visits, 2,600 hospitalizations, and about 500 deaths annually in the U.S. (estimates vary by dataset and year).
Liver failure#
This is acetaminophen’s signature injury.
Acetaminophen is directly hepatotoxic. When metabolized, it produces a toxic byproduct that must be neutralized by glutathione. This depletes glutathione which is such a necessary antioxidant. Once glutathione stores are depleted, the toxic metabolites are able to freely destroys liver cells rapidly and aggressively. With liver defense broken down the body is left open to many attacks that normally would pose no threat.
Liver damage can occur from:
-
Acute overdose
-
Chronic “therapeutic” dosing
-
Combining Tylenol with alcohol, smoking, low water intake, processed foods, and many other things.
-
Taking multiple acetaminophen-containing products
Early symptoms are often mild or misleading, including nausea, vomiting, and abdominal discomfort. As damage progresses, patients develop jaundice, bleeding disorders, confusion, edema, and even death. Many patients do not realize the severity of injury until liver failure is advanced and irreversible. Then doctors often blame it on something other than the cause.
Tylenol is one of the most common over-the-counter drugs capable of causing fatal organ failure on its own.
Intestinal Damage and Bleeding#
Tylenol is falsely promoted as being “easy on the stomach.” While it may not inhibit prostaglandins in the same way as NSAIDs, this does not make it harmless to the gastrointestinal tract.
Acetaminophen toxicity frequently presents with:
-
Severe nausea and vomiting
-
Abdominal pain
-
Gastrointestinal irritation
In real-world use, Tylenol is often taken alongside alcohol, dehydration, poor nutrition, or other medications—all of which increase gastrointestinal and systemic toxicity. Gastrointestinal distress is frequently the first warning sign of poisoning.
Additional Serious Side Effects#
Severe Skin Reactions#
Acetaminophen has been linked to life-threatening skin reactions, including Stevens–Johnson syndrome and toxic epidermal necrolysis. These reactions can occur suddenly and be fatal.
Kidney Damage#
Acetaminophen poisoning can result in acute kidney injury, either alone or in combination with liver failure. Renal damage may persist even after liver recovery.
Increased Risk With Alcohol#
Alcohol dramatically increases acetaminophen toxicity by accelerating production of its toxic metabolite while simultaneously depleting protective glutathione. This combination significantly increases the risk of liver failure, even at doses many people believe are “safe.”
Delayed Toxicity#
One of the most dangerous aspects of Tylenol is delayed injury. People often feel “fine” initially, leading them to to believe the drug is safe while it works silently and at first imperceptibly to weaken the entire system.
Tylenol Toxicity#
An estimated 458 deaths each year are associated with Tylenol overdose. The problem with this statistic is that it reflects only deaths formally concluded to have been caused by Tylenol. There are thousands more deaths in which no association is made, despite Tylenol use being a causal factor. Tylenol is actively used as a suicidal weapon because it is so deadly, yet suicide by Tylenol is not included in these statistics.
Each year, approximately 56,000 people visit the emergency room and 26,000 are hospitalized for Tylenol overdose.
In 1977, even the corrupt FDA was forced to acknowledge the severe toxicity of this drug. They stated that it was “obligatory” to place a warning indicating that Tylenol causes “severe liver damage,” up to and including liver failure. What absolutely astonishes me is that there is valid proof that Tylenol causes liver damage, and millions of people take it regularly without a second thought, yet a single unsubstantiated claim that comfrey causes liver damage leads the FDA to ban it and instills fear in the public. To learn more about the lies surrounding comfrey, watch on The Truth about Comfrey Toxicity
Tylenol is such a serious threat that McNeil has funded the production of an antidote to this poison. But do not mistake this for actual concern for human life. The company has repeatedly and aggressively fought against safety warnings, restrictions on use, and any measures intended to protect Tylenol users. Tylenol is a billion-dollar drug, so it is no surprise that honesty is not their priority.
Many medications contain the toxic compound acetaminophen, meaning you may be ingesting a lethal cumulative dose without realizing it. Acetaminophen overdose is the leading cause of calls to Poison Control Centers, accounting for over 100,000 calls each year.[9]Acetaminophen and the U.S. acute liver failure study group: Lowering the risks of hepatic failure
Acetaminophen hepatotoxicity far exceeds all other causes of acute liver failure in the United States and accounts for nearly 50% of all acute liver failure cases nationwide. [10]Acetaminophen‐induced acute liver failure: Results of a United States multicenter, prospective study[11]Acetaminophen and the U.S. acute liver failure study group: Lowering the risks of hepatic failure
What to do about Tylenol Poisoning / Overdose#
Immediately contact Poison Control and seek medical attention. In the United States, call 1-800-222-1222 without delay.
Activated charcoal should be administered as soon as possible and taken every hour until a physician can be seen. Evidence shows that “those who had been given activated charcoal were significantly less likely to have probable or high-risk concentrations”[12]Activated Charcoal Reduces the Need for N-Acetylcysteine Treatment After Acetaminophen (Paracetamol) Overdose
Another treatment commonly used is gastric lavage, also known as stomach pumping. While it can be beneficial on its own, research indicates that “gastric lavage, in addition to activated charcoal, did not further decrease the risk”[13]Activated Charcoal Reduces the Need for N-Acetylcysteine Treatment After Acetaminophen (Paracetamol) Overdose – In plain terms, activated charcoal is as effective as stomach pumping.
Although medical care should always be sought in cases of poisoning, you owe it to yourself to begin administering activated charcoal immediately. It is a well-established and safe protocol with proven benefits and no added risk.
Do not consume soda, beer, or any form of alcohol if acetaminophen poisoning is suspected. Alcohol significantly increases the risk of toxic liver failure.
Alternatives to Tylenol#
Anti-Inflammatory – Tylenol and Advil work by blocking the formation of inflammation, which may sound beneficial to those unfamiliar with how the body functions. Inflammation is a natural and necessary healing process. Simply suppressing it will always create problems later. Natural anti-inflammatory herbs do not merely block inflammation; they address the underlying cause and actively resolve inflammatory processes rather than shutting down the body’s response.
Ginger – An exceptional natural anti-inflammatory that works on multiple systems of the body simultaneously. Ginger not only breaks down inflammation but also reduces excess acidity in the stomach and joints while calming and protecting the digestive tract. Most importantly, it causes no harm to the liver. Ginger has been shown to be “as effective as betamethasone” for inflammation, without causing damage to the body.[14]A Synoviocyte Model for Osteoarthritis and Rheumatoid Arthritis: Response to Ibuprofen, Betamethasone, and Ginger Extract—A Cross-Sectional In Vitro Study
Ginger is superior to Tylenol because it promotes healing rather than suppressing symptoms. It can be used fresh in foods, soups, and smoothies, or frozen, dried, and prepared as tea. The options are limitless. A ginger, lemon, and cayenne tea frozen into cubes is an excellent anti-inflammatory and immune-supportive remedy.
Turmeric –This powerful spice is remarkable in its ability to combat the cause of inflammation and alleviate pain, particularly pain associated with arthritis and osteoporosis and caused by heavy metal toxicity. Turmeric works by modulating inflammatory pathways and reducing oxidative stress rather than blocking the body’s repair mechanisms. It is usually recommended to be taken with black pepper, which increases its bioavailability by up to 2,000%, making it exponentially more effective. However, the process by which black pepper increases bioavailability is a drug-like mechanism which produces other negative effects. Instead, we recommend to take it with fat which has a similar effect with no downsides. Seeds or nuts are a great fat to choose.
Cayenne – Cayenne is a potent circulatory stimulant, blood equalizer and natural pain reliever. One of its active compounds, capsaicin, works by regulating substance P, a neurotransmitter responsible for transmitting pain signals. Rather than damaging organs, cayenne improves blood flow, supports cardiovascular function, and enhances the delivery of nutrients to injured tissues. It also aids digestion and synergizes powerfully with other anti-inflammatory herbs.
Valerian Root – Valerian is well known for its calming and analgesic effects. It reduces pain by relaxing the nervous system and relieving muscle tension, making it particularly useful for pain rooted in spasms, tension, or nerve irritation. Unlike pharmaceutical painkillers, valerian does not stress the liver or kidneys and supports restorative sleep, which is critical for healing.
Magnesium – Magnesium is an essential mineral involved in hundreds of enzymatic reactions in the body. It plays a critical role in muscle relaxation, nerve signaling, and inflammation regulation. Magnesium deficiency is strongly associated with chronic pain, headaches, muscle cramps, and joint stiffness. Supplementing magnesium reduces inflammatory markers and supports cellular repair rather than masking pain. Magnesium should be either acquired from plants or be applied topically.
Cat’s Claw – Cat’s Claw is a powerful anti-inflammatory and immune-modulating herb traditionally used for arthritis and inflammatory joint disorders. It works by reducing inflammatory cytokines through modulation and supporting immune balance. Rather than suppressing the immune system, it helps regulate excessive inflammatory responses while promoting tissue repair. It is also a powerful herb for things like Lyme disease.
Boswelia – Boswellia, also known as Indian frankincense, is another very effective natural anti-inflammatory agents. It inhibits inflammatory enzymes responsible for joint degeneration while protecting cartilage and connective tissue. Boswellia is particularly effective for osteoarthritis, rheumatoid arthritis, and inflammatory bowel conditions, without causing any gastrointestinal or liver damage.
White Willow Bark – White Willow Bark is the original source from which aspirin was derived, but in its natural form it works more intelligently with the body. It provides pain relief by reducing inflammation gradually and sustainably, without the harsh effects associated with synthetic salicylates. Unlike Tylenol, it does not cause liver toxicity and supports long-term pain management rather than short-term suppression.
These alternatives do not poison the liver, do not shut down natural healing mechanisms, and do not create dependency. They work with the body, not against it.
References