- Why Delayed Cord Clamping
- Maternal Medications: The Iatrogenic Creation of Vitamin K Deficiency
- Synthetic Oxytocin (Pitocin)
- Tocolytics
- Magnesium Sulfate
- Antiemetics and Anxiolytics
- Glucocorticoids for Fetal Lung Maturation
- Anticonvulsant Medications
- Anticoagulant Medications (Warfarin and Coumarins)
- Antituberculosis (antibiotic) Medications
- Cephalosporin Antibiotics
- The Cascade of Drug Intervention That Creates the Crisis
- What These Drugs Actually Destroy
- The Bias
- Historical
- The Science Is Very Clear
- The Definition of "Delayed" Matters
- Statistical Manipulation in Research
- Why Babies Are Born with Low Vitamin K
- The Stem Cell Puzzle Piece
- The Digestive System
- Historical Medical Skepticism
- The Cancer Connection
- Why This Continues
You can view drug details for the Vitamin K1 Injection here
Proponents of the Vitamin K shot emphasize that delayed cord clamping does not significantly increase Vitamin K transfer to the newborn. This is true but it’s not the gotcha they may think it is. Nature does not intend for babies to receive what they are not yet ready to process, as their gut/digestive systems are not fully developed at birth. In a peer-reviewed paper published in the Journal Pediatric Blood & Cancer, the authors state that “Vitamin K deficiency bleeding (VKDB) can occur in neonates and infants due to low placental transfer.”[1]International Perspectives on Vitamin K Deficiency Bleeding in Infants: A Cross-Sectional Questionnaire-Based Survey. This is a very ironic statement to me. While proponents highlight that Vitamin K does not transfer significantly through the placenta, this prestigious journal attributes VKDB to low placental transfer. Shouldn’t we be asking what causes this low placental transfer in the first place?
Why Delayed Cord Clamping#
It is a well-established fact that delayed cord clamping saves lives, yet there is no widespread push to implement this practice—which has zero downsides and costs nothing. Instead, the medical establishment aggressively promotes an injection that carries a black box warning. Why? If saving infant lives is truly the priority, we should see a universal push for delayed cord clamping, which costs nothing except the doctor’s time—but time is money. Is it then all really only about money?
Recent and historical evidence reveals that placental transfusion, facilitated by delayed cord clamping (DCC), reduces infant death and the need for blood transfusions in preterm infants without any harm. Even a brief delay in clamping shows improved survival and well-being, but waiting at least two minutes or until the cord stops pulsating (and often turns white/flat) maximizes the placental transfusion of blood, iron, stem cells, and oxygen to the baby. At least three major benefits from DCC contribute to reduced mortality in preterm infants: benefits from the components of blood, assistance from the continued circulation of blood, and the essential mechanical interactions that result from the enhanced volume of blood. The enhanced blood volume generates mechanical forces within the microcirculation that support the newborn’s metabolic and cardiovascular stability, greatly improving both short and long-term organ health.[2]
Early cord clamping denies the newborn a full quota of iron-rich red blood cells as well as valuable stem cells for regeneration, repair, and seeding of a strong immune system.[2] These stem cells are designed by nature for regeneration and repair. Nature by design has provided the answer, but we have a medical system built around profit—prioritizing the planning and scheduling of births (which also explains our epidemic of unnecessary cesarean sections) instead of waiting for nature’s timing. The use of forceps causes internal bleeding, maternal medications destroy the quality of blood supply to the child, and quick clamping—all of these factors have produced a perceived need for Vitamin K shots. We caused the problem, then offered a black box warning solution.
Maternal Medications: The Iatrogenic Creation of Vitamin K Deficiency#
The medical establishment’s own interventions have manufactured much of the perceived “need” for universal Vitamin K injections. Numerous maternal medications interfere with vitamin K stores or function, including enzyme-inducing anticonvulsants such as phenytoin, phenobarbital, and carbamazepine, antituberculosis drugs like rifampin and isoniazid, certain cephalosporin antibiotics, and anticoagulants including warfarin and other coumarin derivatives(5)(6) These drugs cross the placenta and fundamentally disrupt the baby’s natural birth recovery system—not merely by depleting vitamin K, but by sabotaging the delicate balance nature designed for newborn repair and regeneration.
Before examining specific drugs, we must understand what they destroy. Nature designed babies with intentionally thin blood and low clotting factors for the first few days of life. This is not a defect—it is the mechanism that allows stem cells from delayed cord clamping to flow freely through the baby’s circulation, reaching any tissue damaged during birth to perform regeneration and repair. These stem cells cross the blood-brain barrier and can access every organ. This naturally thinner blood is essential for these elements to move quickly and effectively. Vitamin K, by contrast, serves only a narrow function: it supports the formation of clotting proteins, whereas the stem cells and biological factors from the placenta participate in repairing and restoring tissues—functions that Vitamin K does not perform.
Maternal medications sabotage this system in two primary ways:
- Depleting or interfering with vitamin K metabolism, forcing the baby’s blood to become even thinner than nature intended creating high risk of bleeding and even death
- Disrupting clotting factor production and blood composition in ways that make the blood incompatible with the stem cell circulation and repair that should occur naturally
In both cases, the medical system creates a crisis, then uses that manufactured crisis to justify injecting all babies—even those with no objective risk.
Synthetic Oxytocin (Pitocin)#
Pitocin is routinely administered during labor to induce or augment contractions in at least 50% of births in the United States. While synthetic oxytocin does not directly deplete vitamin K, it fundamentally disrupts the quality of placental perfusion and the physiological environment the baby is born into. Pitocin-induced contractions are stronger, longer, and more frequent than natural contractions, reducing the rest periods between contractions during which the placenta refills with oxygenated blood. This creates a iatrogenic state of repeated fetal hypoxia—oxygen deprivation—which stresses the baby and reduces the oxygen-carrying capacity of the blood available through delayed cord clamping.
Hypoxic stress increases the metabolic demand on the newborn and interferes with the baby’s ability to utilize stem cells effectively for post-birth repair. Pitocin, throughout the excessive uterine contractions, also increases the risk of placental abruption, fetal distress, jaundice, and admission to neonatal intensive care—all of which correlate with elevated bleeding risk, increased interventions, including the perceived need for aggressive vitamin K administration. Furthermore, it often leads to an increased likelihood of postpartum hemorrhage in the mother, which then triggers administration of additional hemostatic drugs and a cascade of additional interventions, including epidural anesthesia and the barbaric forceps delivery, each carrying their own risks to the newborn’s blood quality and stem cell function—all of which creating problems that often require additional pharmaceutical solutions.
The drugging of the mother in birth through synthetic oxytocin creates an environment where the baby is born under duress, with compromised oxygenation and altered physiology—which contributes to factors associated with severe bleeding in infants.
Tocolytics#
The medical profession is obsessed with messing with nature. If they aren’t administering Pitocin to increase contractions, they will administer tocolytic medications to delay preterm labor, including nifedipine (a calcium channel blocker), indomethacin (a prostaglandin synthesis inhibitor), and terbutaline (a beta-agonist), all cross the placenta and affect fetal physiology.
Indomethacin in particular has been associated with neonatal complications including altered platelet function and increased bleeding risk. While these medications are typically discontinued before delivery, their effects on fetal physiology—including potential alterations to the coagulation system—may persist into the immediate neonatal period.
Magnesium Sulfate#
Magnesium sulfate is administered intravenously during labor for seizure prophylaxis in women with preeclampsia or eclampsia, and for neuroprotection in preterm births. While magnesium sulfate does not directly interfere with vitamin K metabolism, it crosses the placenta freely and causes neonatal hypermagnesemia,(19) which manifests as hypotonia, respiratory depression, and poor feeding.
These effects compound the challenges facing a newborn whose vitamin K stores are already limited. Respiratory depression reduces hepatic oxygenation and impairs clotting factor synthesis. Poor feeding delays gut colonization with vitamin K-producing bacteria and reduces intake of the small amounts of vitamin K present in colostrum and early breast milk. The result is a neonate whose vitamin K status is compromised by well-intentioned but foolish and unnecessary maternal treatments.
Antiemetics and Anxiolytics #
Medications to manage nausea and anxiety during labor, including ondansetron (Zofran), metoclopramide (Reglan), promethazine (Phenergan), and benzodiazepines such as midazolam and lorazepam, are frequently administered and readily cross the placenta.
Benzodiazepines in particular cause neonatal sedation, hypotonia, hypothermia, and feeding difficulties—a constellation known as “floppy infant syndrome.”(20) These drugs impair the newborn’s ability to initiate breastfeeding, which is the natural mechanism for receiving vitamin K in the early postnatal period as the vitamin K pathways fully develop. By disrupting feeding, these medications create a vitamin K deficit where none would have existed.
Ondansetron and metoclopramide, while generally considered safer than benzodiazepines, still cross the placenta and can affect neonatal gastrointestinal function and feeding behavior. “We found that ondansetron rapidly crosses the placental barrier, it undergoes significantly slower neonatal clearance in the first day of life.“(21) Any medication that interferes with the establishment of normal feeding patterns indirectly compromises vitamin K status.
Glucocorticoids for Fetal Lung Maturation#
Betamethasone and dexamethasone are routinely administered to women at risk of preterm birth to accelerate fetal lung maturation. While these medications can reduce respiratory distress syndrome, they cross the placenta and have documented effects on fetal and neonatal physiology, including suppression of the hypothalamic-pituitary-adrenal axis, alterations in glucose metabolism, and changes in blood pressure regulation.
Emerging evidence suggests that antenatal corticosteroids may also affect neonatal coagulation. Studies have found altered platelet function and changes in clotting factor levels in newborns exposed to antenatal corticosteroids. While the clinical significance is still being investigated, the possibility that these widely used medications affect the very system that vitamin K injections are meant to support deserves far more attention than it has received. At the very least these drugs stress an immature infant body.
Anticonvulsant Medications#
Anticonvulsants administered during pregnancy enter the fetal circulation and cause increased oxidative degradation of vitamin K. Hemorrhage in newborns related to anticonvulsant use generally occurs very early, within the first 24 hours, probably due to increased degradation of vitamin K—the most severe and dangerous form of bleeding.
More than 40 reports have linked neonatal bleeding with maternal anticonvulsant therapy.(7)(9) Enzyme-inducing anticonvulsants such as phenobarbital, phenytoin, and carbamazepine cross the placenta and may induce degradation of vitamin K(8)(9).
Evidence also suggests that anticonvulsant drugs not only affect vitamin k metabolism but also folic acid and often results in conditions such as MTHFR mutation.
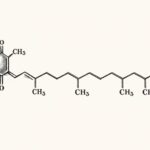
Anticoagulant Medications (Warfarin and Coumarins)#
Warfarin and other coumarin derivatives represent perhaps the most devastating example of medically-induced fetal harm, when it comes to this subject. Warfarin blocks the enzyme Vitamin K epoxide reductase, which is responsible for activating vitamin K during vitamin K recycling, preventing the activation needed for blood clotting factors and the pro-bone-building hormone osteocalcin(10) Warfarin therapy during pregnancy is associated with increased risk of embryopathy, particularly between gestational weeks 6 and 12, as well as fetal intraventricular hemorrhage and cerebral microbleedings that can result in microencephaly and mental retardation.(11)
Studies reviewing 979 pregnancies involving coumarin exposure found that only 689 children were born alive, with skeletal anomalies indicative of coumarin embryopathy occurring in 6% of those exposed throughout pregnancy(12). Approximately 6% of newborns exposed to maternal coumarin intake develop coumarin embryopathy, with 80% showing skeletal anomalies and 45% displaying central nervous malformations(13). Among women administered coumarins during pregnancy, 22% experienced miscarriage(13).
Antituberculosis (antibiotic) Medications#
Antituberculosis drugs, particularly rifampin and isoniazid, are known to cause hemorrhagic disease of the newborn.(14)(6). Rifampin is known to interfere with vitamin K metabolism, leading to hypoprothrombinemia, with the pathogenesis considered to be both disturbed absorption of cvitamin K from the intestine and interference with vitamin K metabolism.(15). Rifampin influences vitamin K synthesis and is associated with increased risk of hemorrhagic complications in both mother and newborn(16).
Cephalosporin Antibiotics#
If the mother has taken cephalosporin antibiotics, the risk of hemorrhagic disease in the newborn is increased(17). Ceftriaxone and other third-generation cephalosporins decrease the activity of hepatic microsomal carboxylase and disrupt vitamin K metabolism preventing activation, which can lead to coagulation disorders and bleeding(18). These antibiotics inhibit carboxylation of prothrombin, and deficient carboxylation results in reduced calcium binding and lower efficiency of prothrombin(18).
Intrapartum antibiotic prophylaxis for Group B Streptococcus (GBS) colonization is administered to approximately 30% of women during labor in the United States. The most commonly used antibiotics—penicillin, ampicillin, and cefazolin—all cross the placenta and reach therapeutic levels in fetal circulation.
Moreover, intrapartum antibiotics disrupt the normal microbial colonization of the newborn gut, delaying the establishment of vitamin K-producing bacteria. This effect persists for weeks after birth, extending the window during which the infant depends entirely on dietary vitamin K intake or stored reserves.
Cephalosporins antibiotics containing side chains of N-methylthiotetrazole, including latamoxef, cefmenoxime, cefoperazone, cefotetan, and cefamandole, or methyl-thiadiazole like cefazolin, all cause transient plasma appearance of vitamin K epoxide in response to vitamin K administration, indicating they are inhibitors of hepatic vitamin K epoxide reductase. After vitamin K is given, these drugs cause a rise in vitamin K epoxide in the blood, which shows that they inhibit hepatic vitamin K epoxide reductase, an enzyme the liver uses to recycle vitamin K. God designed the baby with the ability to recycle the small amounts of vitamin K it receives, however, this ability is neutralized by many drugs. Again, this creates the crisis that vitamin K injection is necessary for.
Third-generation cephalosporins including ceftriaxone also reduce the activity of liver enzymes (microsomal carboxylase) needed for proper vitamin K metabolism. This interference prevents normal carboxylation of prothrombin, a step required for it to bind calcium and function effectively in blood clotting. When carboxylation is impaired, prothrombin becomes less efficient, increasing the risk of bleeding.
Even infants who receive vitamin K at birth can develop life-threatening deficiency if exposed to cephalosporins. This is how dangerous they are. A 3-month-old infant who had received vitamin K at birth developed severe bleeding during maternal ceftriaxone treatment combined with prolonged diarrhea, demonstrating that these antibiotics can overwhelm even the massive prophylactic vitamin K. This raises a critical question: if the injection doesn’t even protect against later cephalosporin exposure, why is it given universally rather than reserving it for actual emergencies?
Notice the pattern. Modern medicine intervenes with pharmaceutical agents during pregnancy. These drugs cross the placenta, destroy the baby’s vitamin K stores or interfere with vitamin K metabolism, and create bleeding disorders. The medical establishment then uses these drug-induced complications as justification for universal prophylaxis in all newborns—including the vast majority who were never exposed to these medications and would not have had any bleeding problems.
We prescribe anticonvulsants that induce fetal enzymes to degrade vitamin K. We keep pregnant women on warfarin despite knowing it causes embryopathy and fetal death. We give antituberculosis drugs that interfere with vitamin K synthesis. We administer antibiotics liberally that inhibit vitamin K recycling. We create the bleeding. We manufacture the crisis. And then we write clinical guidelines mandating injections for all infants to solve the catastrophe we engineered. And our solution? A black box warning injection which will create more conditions that other drugs will be prescribed for. There is definitely no conspiracy here.
What becomes clear when examining labor and delivery medications as a category is that virtually every pharmaceutical intervention during birth has the potential to affect neonatal vitamin K status, either directly through interference with vitamin K metabolism, or indirectly through effects on respiratory function, hepatic perfusion, feeding behavior, or gut colonization.
The Cascade of Drug Intervention That Creates the Crisis#
More insidiously, these interventions tend to cluster. A mother who receives Pitocin for labor augmentation is more likely to need an epidural for pain management. Epidural anesthesia increases the likelihood of prolonged labor, which increases the likelihood of additional Pitocin, antibiotic administration, and barbaric forceps delivery. Each intervention creates conditions that justify the next, often culminating in a newborn who has been exposed to a pharmaceutical cocktail in the hours before birth—then declared deficient and in need of yet another injection.
What These Drugs Actually Destroy#
Understanding what these medications truly sabotage requires understanding God’s design. A baby is born with a sophisticated and intelligent system for surviving and recovering from birth trauma:
- Intentionally thin blood with low vitamin K for the first few days of life as an essential feature that allows maximum circulation efficiency
- Stem cells from delayed cord clamping are designed to circulate freely while blood is thin, crossing the blood-brain barrier and reaching any tissue damaged during birth
- The ability of these stem cells to cross the blood-brain barrier and reach any damaged tissue
- A built-in repair mechanism that works precisely because blood is thin enough for stem cells and growth factors to move quickly to areas of damage
- A vitamin K recycling system that is sufficient for normal newborn needs, designed to work with the small amounts of vitamin K the baby receives through delayed cord clamping and early breast milk
- A transitional system designed to first prioritize tissue repair as the newborn develops
Maternal medications destroy this system in multiple compounding ways:
First Level of Destruction: Direct Vitamin K Depletion and Metabolism Interference#
- Anticonvulsants (phenytoin, phenobarbital, carbamazepine) cause increased oxidative degradation of vitamin K, forcing the baby’s vitamin K stores to pathologically low levels)
- Anticoagulants (warfarin, coumarins) block the enzyme vitamin K epoxide reductase, preventing the recycling of vitamin K and causing accumulation of inactive vitamin K epoxide

- Antituberculosis drugs (rifampin, isoniazid) interfere with both vitamin K absorption and metabolism, disrupting the gut-liver balance that would normally maintain adequate vitamin K levels
- Cephalosporin antibiotics (ceftriaxone, cefazolin) inhibit vitamin K epoxide reductase and decrease hepatic microsomal carboxylase activity, blocking both vitamin K recycling and the activation of clotting factors
The result is that babies cannot utilize the stem cells from delayed cord clamping effectively. The birth trauma cannot be repaired efficiently. The natural system is sabotaged. And the medical establishment then claims the baby was “deficient by design” and needs pharmaceutical intervention to survive.
The Bias#
If vitamin K deficiency bleeding were truly a universal problem of a flawed design, we would expect to see it relatively equally distributed across populations. We don’t. The reported incidence of VKDB in infants of mothers who have received anticonvulsants, antituberculosis drugs, or anticoagulants without vitamin K supplementation is between 6 and 12 percent. This means that 88-94% of even babies exposed to these drugs do NOT develop VKDB, even without intervention.
For babies not exposed to these harmful medications, the rate is even lower—vanishingly rare. Yet we inject everyone. Why? Because it is more profitable to create a universal market than to practice targeted medicine and promote harmless practices such as delayed cord clamping.
There are remarkably few honest studies that directly measure the real-world difference between infants who receive prophylactic vitamin K injections and those who do not. In one of the rare large-scale analyses, 1.5 million births were examined. In that dataset, the incidence of VKDB among infants who did not receive vitamin K was 4.27 cases per 100,000 births.(22) Expressed as percentages, this is 0.00426% in the untreated group versus 0.000419% in the vitamin-K-injected group. (The highest documented rate in a large data sample is 12.4 cases per 100,000 births—nowhere even remotely close to the 1,600 per 100,000 figure promoted by mainstream media.)
When these numbers are translated into meaningful terms, the result is eye-opening. The number needed to treat (NNT) to prevent a single case of VKDB is 26,030 infants. In other words, 26,030 newborns must be injected to prevent one case. The remaining 26,029 infants receive no objective benefit, because they would never have developed VKDB regardless.
The scientific question is: how many of those 26,000 injected infants are harmed by the drug’s black-box-warned risks? That is the purpose of risk–benefit analysis. Claims that vitamin K shots “save lives” are meaningless unless treated and untreated populations are compared and harms in the treated group are counted. Without that, there is no scientific basis for declaring lives saved.
Historical #
This concept is not new. We have known this for hundreds of years, and nature itself tells us when to clamp and cut the cord. Erasmus Darwin (Charles Darwin’s grandfather) wrote in 1801:
“Another thing very injurious to the child, is the tying and cutting of the navel string too soon; which should always be left till the child has not only repeatedly breathed but till all pulsation in the cord ceases. As otherwise the child is much weaker than it ought to be, a portion of the blood being left in the placenta, which ought to have been in the child.”
The Science Is Very Clear#
Multiple randomized controlled trials have reported that waiting to clamp the umbilical cord for at least 60 seconds after birth results in an average 30% decrease in the incidence of death for preterm infants. Yet the most recent evidence on DCC shows that current standard recommendations to delay clamping for 30 to 60 seconds may be insufficient—longer delays result in fewer deaths.[2]
One study found decreased mortality by 36 weeks postmenstrual age for those who received delayed cord clamping, with a relative risk of 0.29 (95% CI 0.49 to 0.97, P=0.03).[3] This means babies with delayed clamping were 71% less likely to die by 36 weeks compared to babies who did not receive delayed clamping. This statistic has a 97% probability of accuracy—more significant than most studies used to justify the Vitamin K shot. Noteworthy is that researchers post hoc adjusted the delayed clamping statistics but not the early clamping statistics, which is highly irregular.
Another study found that delayed cord clamping significantly reduced hospital mortality compared to early clamping in preterm infants, with a relative risk of 0.69 (95% CI 0.52-0.91, p=0.009).[3] This represents a 31% reduction in the risk of death. To put this in perspective: if hospitals switched completely to delayed cord clamping based on this statistic, we could expect to see 3,030 preterm babies survive to hospital discharge who currently die. Compare this to the Vitamin K shot, which is estimated to save 1-2 deaths per 100,000 births from late VKDB, and approximately 160 deaths per 100,000 births total. Delayed clamping—which has no black box warning and zero downsides could save approximately 1,793% more lives than the Vitamin K shot. We can argue, with significant supporting evidence, that these 160 lives allegedly saved by the Vitamin K shot would either be saved by delayed cord clamping or by keeping mothers off medications in almost all cases. And we have not even factored in deaths caused by the Vitamin K shot, either directly or indirectly.
The Definition of “Delayed” Matters#
One systematic review by the Cochrane Collaboration found low quality evidence for delaying clamping by only 30 seconds. Some have used this to suggest that delayed clamping is not significantly important, but that conclusion is backwards. All studies delaying 60 or more seconds show clear benefits, indicating that 30 seconds does not qualify as true “delayed clamping.” Only 60 or more seconds is delayed, and ideally it should be at least 120 seconds.
Statistical Manipulation in Research#
Unfortunately, some research appears to purposely and intentionally construe facts to present a story that fits a narrative rather than simply reporting findings honestly. A prime example is an article published in the New England Journal of Medicine. In their results and conclusion, they present a false narrative based on the twisting of data, stating:
“There was no significant difference in the incidence of the primary outcome between infants assigned to delayed clamping (37.0%) and those assigned to immediate clamping (37.2%). Among preterm infants, delayed cord clamping did not result in a lower incidence of the combined outcome of death or major morbidity at 36 weeks of gestation than immediate cord clamping.”[4]
The problem is that this is not what the study actually found. They created two outcome groups to confuse the issue. Immediately after this misleading statement, they reveal the fact:
“The mortality was 6.4% in the delayed-clamping group and 9.0% in the immediate-clamping group.”[4]
But they adjusted this result post hoc to reach their desired conclusion. How do we know this? Because they explicitly state: “Our analysis plan specified no adjustment.” The decision to apply a post hoc statistical penalty specifically to the mortality comparison—after observing a significant difference favoring DCC—introduces direct inconsistency in their stated and planned analytical approach. No equivalent adjustment was applied to other secondary outcomes that might have favored immediate cord clamping. This post hoc adjustment violates their pre-specified “no adjustment” plan and introduces clear and unfair bias.
The authors adjusted for 13 secondary outcomes, but mortality was only one of them. The Benjamini-Hochberg procedure controls the false discovery rate across all tested hypotheses, which is conservative when many outcomes are unrelated. Mortality is a distinct, clinically paramount outcome—not just one of many equivalent endpoints. Adjusting it alongside less critical outcomes inappropriately dilutes its significance.
Why Babies Are Born with Low Vitamin K#
Consider how nature is determined to ensure Vitamin K levels remain low in newborns:
- There is little transfer of Vitamin K1 from mother to baby via the placenta
- Babies are not born with enough bacteria in their intestines to make Vitamin K2
- Breast milk has low levels of Vitamin K compared with other mammal milk, such as cow’s milk, or fortified infant formula (breastmilk contains only 1-9 mcg/L compared with formula at 53-66 mcg/L)*
*Vitamin K1 content in breastmilk can be increased by increasing maternal dietary intake of vitamin k rich foods such as greens(17)
Either nature has made a catastrophic error, or there is a good reason why babies are born with lower levels of Vitamin K than adults.
Vitamin K levels are virtually undetectable in umbilical cord blood, suggesting that babies are not receiving any significant Vitamin K from their mothers via placental transfer. I believe this is normal and intentional, especially when we consider babies are born with their own built-in system to protect against and repair damage and bleeding in their organs—thanks to umbilical stem cells. However, these stem cells can only travel around the body while the blood remains thin and when the umbilical cord is left intact after birth (delayed cord clamping). It was not until the late 1980s that cord stem cells were discovered, a few decades after Vitamin K prophylaxis had become routine for all newborns.
The Stem Cell Puzzle Piece#
Any fetus that endures the journey down the birth canal can incur damage in any part of the body, including the brain, and needs a built-in repair mechanism. Modern medicine assumes that the only answer must be Vitamin K. However, stem cells from the placental transfer cross the blood-brain barrier and can go anywhere in the body. This is God’s design. There are actually three solutions. The second is that naturally, in the first few days, a baby’s blood clotting factors are intentionally lower than normal.
Pediatricians consider this a “defect” and want to give Vitamin K, which results in blood nearly 100 times thicker than an adult’s. This Vitamin K injection, they claim (just as they say immediate cord clamping is safe and normal while delayed cord clamping is an “unproven intervention”), is necessary because the baby was not designed correctly, and without it, the baby “could bleed to death.”
It is no coincidence that the Vitamin K syringe sits right alongside the cord clamp and scissors.
But there is an unanswered question: Why are blood clotting factors in babies low in the first few days after birth? Why does a baby have much thinner blood as a result?
A logical hypothesis: thinner blood allows freer and quicker access of cord blood stem cells to any part of the body damaged during birth. Why should stem cells have to fight through a baby’s blood that is now 100 times thicker than any adult’s, courtesy of another needle? An injection that contains a toxic preservative that kills babies.
The Digestive System#
To absorb Vitamin K, we must have a functioning biliary and pancreatic system. An infant’s digestive system is not fully developed at birth, which is why we give babies breast milk and delay solids until they are at least six months old, and why breast milk contains only a small amount of Vitamin K, but a highly absorbable form. Too much Vitamin K taxes the liver which is not yet able to utilize it properly, especially in extreme doses, and it can cause brain damage, among other problems. The neonatal liver is immature with respect to prothrombin synthesis,(17) this is why a massive dose is given. As the baby ages and the digestive tract, mucosal lining, gut flora, and enzyme functions develop, the baby can process more Vitamin K. Low levels of Vitamin K at birth make sense in the light of a developing baby.
A newborn has low levels of Vitamin K because its intestines are not yet colonized with bacteria needed to synthesize it, and the “Vitamin K cycle” is not fully functional in newborns. It might seem logical to bypass the gut and inject Vitamin K directly into the muscle—except the baby’s kidneys are not fully functional either.
Babies are born with low levels of Vitamin K compared to adults, but this level is still sufficient to prevent problems. Vitamin K prophylaxis is not necessarily needed in most cases. Several clinical observations support the hypothesis that children have natural protective mechanisms that justify their low Vitamin K levels at birth. We should probably figure out why that is before we “inject now and worry about it later,” especially with a black box product.
Historical Medical Skepticism#
As early as April 17, 1977, an article in one of the world’s most esteemed medical journals, the Lancet, discredited the policy of routine Vitamin K injections: “We conclude that healthy babies, contrary to current beliefs, are not likely to have a vitamin K deficiency… the administration of vitamin K is not supported by our findings,” Van Doorm et al stated. Twenty-one peer-reviewed reports published in prominent medical journals have concurred that policies mandating universal injection of newborn babies are not based on sound science.
Since 1985, the medical profession has known that oral Vitamin K raises blood levels 300 to 9,000 times higher than normal. Injectable Vitamin K results in Vitamin K levels 9,000 times thicker than adult blood.
Baby’s blood thickened with Vitamin K creates a situation where stem cells have to move through sludge rather than smooth-flowing, optimally circulated blood vessels full of blood that allows stem cells easy access anywhere. Perhaps one day it will dawn on the medical profession that not only are cord blood stem cells important and useful to the newborn baby, but that stem cells need thin blood for a reason. God designed the entire system perfectly.
The Cancer Connection#
The British Journal of Cancer published “Factors associated with childhood cancer” by J. Golding et al in 1990. The report indicated that universally administered intramuscular Vitamin K injections significantly increase children’s chances of developing childhood cancer. A follow-up study published two years later in the British Medical Journal reinforced the findings of the previous study. The authors commented conservatively, as is scientific custom, but parents concerned about their babies’ health will read “danger” between these lines:
“The only two studies so far to have examined the relation between childhood cancer and intramuscular vitamin K have shown similar results and the relation is biologically plausible. The prophylactic benefits against haemorrhagic disease are unlikely to exceed the potential adverse effects from intramuscular vitamin K.”
We have already established that delayed cord clamping could save 3,030 lives per 100,000 preterm births, while Vitamin K injections save only about 160. That alone exposes a catastrophic imbalance in medical priorities. But the problem goes far deeper. The evidence now indicates that the risk profile of the Vitamin K injection itself likely outweighs any theoretical benefit it provides. This is precisely why Van Doorm, in 1977, warned that the universal administration of Vitamin K to newborns was not grounded in solid scientific evidence. That warning has never been responsibly resolved or debunked.
Why This Continues#
Why is Vitamin K relentlessly pushed on parents and their newborns? Why are mothers and fathers made to feel irresponsible—even dangerous—if they refuse it? Why are they almost never told that this injection carries a black box warning, the FDA’s highest level of drug risk disclosure? Because pharmaceutical companies do not like to lose revenue. Doctors do not like to be challenged. And the American Academy of Pediatrics has demonstrated that it does not place the highest priority on the actual biological interests of infants or the informed consent of parents. If it did, delayed cord clamping would be universally promoted and aggressively protected.
We have created a medical system that interrupts natural processes, creates problems through intervention, and then sells solutions to the problems we as humans have caused. Delayed cord clamping costs nothing, has no side effects, provides stem cells for repair and regeneration, delivers a full quota of iron-rich blood, reduces mortality by 31-71%, and works with the baby’s natural design. Yet it is not universally practiced because it requires patience—and patience does not generate revenue. In contrast, the routine vitamin K injection has been converted into a global market generating approximately $250–$400 million every year, transforming a naturally sufficient newborn system into a recurring revenue model—while a free, life-preserving practice like delayed cord clamping remains marginalized precisely because it cannot be sold.
References
- International Perspectives on Vitamin K Deficiency Bleeding in Infants: A Cross-Sectional Questionnaire-Based Survey. https://onlinelibrary.wiley.com/doi/10.1002/pbc.31889
- How Delayed Cord Clamping Saves Newborn Lives. https://pmc.ncbi.nlm.nih.gov/articles/PMC12110096/
- Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. https://www.ajog.org/article/S0002-9378(17)31439-4/abstract
- Delayed versus Immediate Cord Clamping in Preterm Infants. https://pubmed.ncbi.nlm.nih.gov/29081267/
- Antenatal drugs affecting vitamin K status of the fetus and the newborn
https://pubmed.ncbi.nlm.nih.gov/8747699/ - Vitamin K Deficiency Bleeding (VKDB) in Neonates and Infants
https://emedicine.medscape.com/article/974489-overview?form=fpf - Neonatal coagulation defect due to anticonvulsant drug treatment in pregnancy
https://pubmed.ncbi.nlm.nih.gov/4189292/ - Hemorrhagic disease of the newborn after maternal anticonvulsant therapy: a case report and literature review
https://pubmed.ncbi.nlm.nih.gov/3065431/ - Does vitamin K prophylaxis prevent bleeding in neonates exposed to enzyme-inducing antiepileptic drugs in utero?
https://pmc.ncbi.nlm.nih.gov/articles/PMC1780148/ - Fetal warfarin syndrome
https://en.wikipedia.org/wiki/Fetal_warfarin_syndrome - Antenatal drugs affecting vitamin K status of the fetus and the newborn
https://pubmed.ncbi.nlm.nih.gov/8747699/ - Embryopathy – Textbook
https://www.sciencedirect.com/topics/nursing-and-health-professions/embryopathy - Vitamin K supplementation during pregnancy for improving outcomes
https://pmc.ncbi.nlm.nih.gov/articles/PMC6481496/ - Haemorrhagic disease of the newborn in the offspring of rifampicin and isoniazid treated mothers
https://pubmed.ncbi.nlm.nih.gov/998222/ - Management of tuberculosis in pregnant women and newborn infants Guideline – Queensland Health
https://www.health.qld.gov.au/__data/assets/pdf_file/0030/444558/tb-guideline-pregnancy.pdf - Rifampicin
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/rifampicin - Vitamin K Deficiency – MSD Manual Professional Edition
https://www.msdmanuals.com/professional/nutritional-disorders/vitamin-deficiency-dependency-and-toxicity/vitamin-k-deficiency - VITAMIN K DEFICIENCY BECAUSE OF CEFTRIAXONE USAGE AND PROLONGED DIARRHOEA
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1440-1754.2011.02090.x - Hypermagnesemia in preterm neonates exposed to antenatal magnesium sulfate
https://pubmed.ncbi.nlm.nih.gov/35373935/ - Neonatal Withdrawal Syndrome: Reproductive Psychiatry
https://www.sciencedirect.com/topics/psychology/neonatal-withdrawal-syndrome - Ondansetron Pharmacokinetics in Pregnant Women and Neonates: Towards a New Treatment for Neonatal Abstinence Syndrome
https://pmc.ncbi.nlm.nih.gov/articles/PMC4325425/ - Vitamin K deficiency bleeding in Great Britain and Ireland: British Paediatric Surveillance Unit Surveys, 1993–94 and 2001–02
https://pmc.ncbi.nlm.nih.gov/articles/PMC2084011/
References